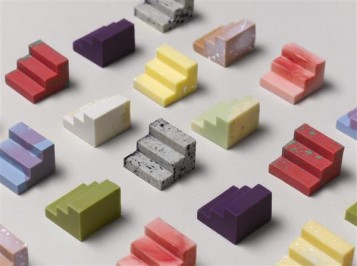
Bioprinting new organs and tissues could make transplants available and affordable for all, but is still decades away. In the meantime, scientists have re-purposed the technology to 3D print biocompatible high-precision silicone implants instead.
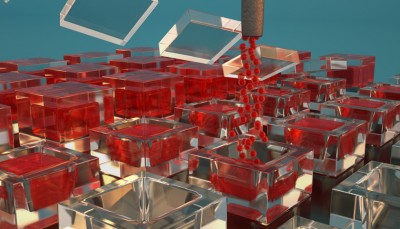
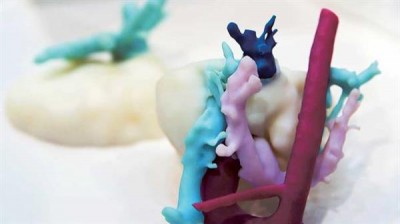
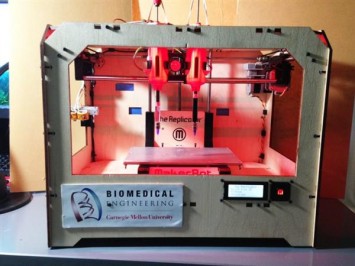
Soft materials like biological material or silicone are difficult to 3D print because they can’t support themselves like the more rigid plastics typically used by 3D printers. In 2015, Tommy Angelini’s lab at the University of Florida developed a new way of 3D printing soft materials by injecting them into a granular gel similar to hand sanitizer that supports them as they are deposited.
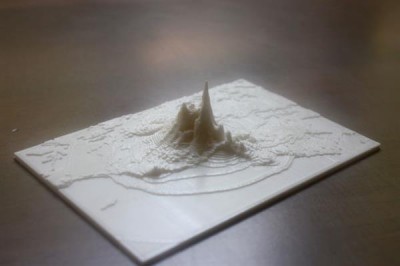
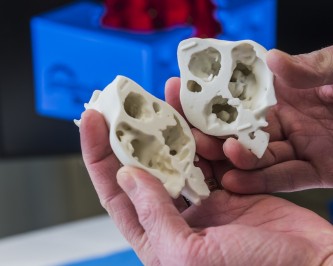
This allowed them to print various shapes using hydrogels, silicone and other polymers, including replicas of organs that allow surgeons to practice before they carry out a procedure. They also managed to print living cells using the method, suggesting it holds promise for bioprinting too.
But while major advances have been made in bioprinting in recent years, it is still decades away from practical medical use. Tech analysts IDTechEx predict the global 3D bioprinting market will be worth $1.8bn by the year 2027, but this growth will be on the back of applications like drug screening and testing and development of cosmetics and other consumer goods.
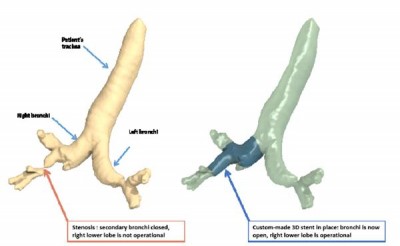
In contrast, silicone is already widely used for medical implants, including things like tubes for draining bodily fluids, catheters, pacemakers and stents designed for the airways. Being able to 3D print these devices could make highly customized implants far cheaper and quicker to produce.
But while the method devised by Angelini and colleagues two years ago was able to print in silicone, its precision and strength were limited. This was due to the fact that the granular gel materials were water-based and thus incompatible with oily silicone inks.
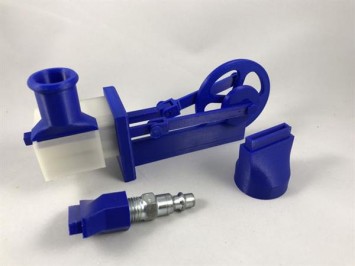
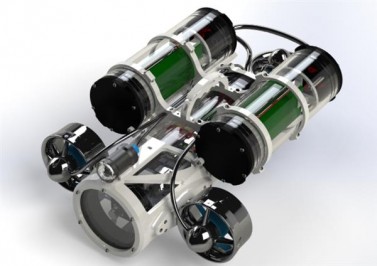
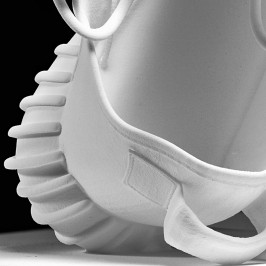
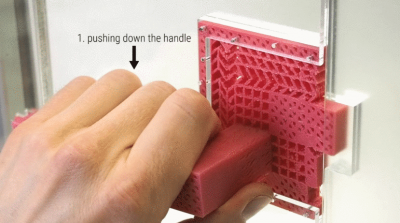
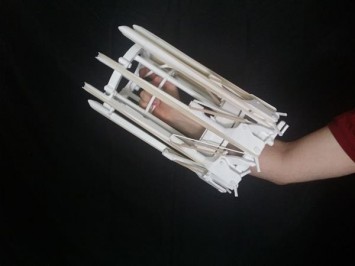
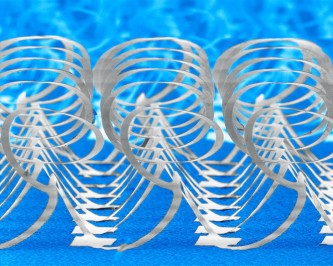
Now the group has created new oil-based gel that allows them to 3D print silicone structures at super high precision that are also highly durable. This has allowed them to create 3D scaffolds, networks of hollow vessels, a functional fluid pump and even a model tracheal implant.
“The reality is that we are probably decades away from the widespread implanting of 3D printed tissues and organs into patients,” Angelini said in a press release.
“By contrast, inanimate medical devices are already in widespread use for implantation. Unlike the long wait we have ahead of us for other 3D bioprinting technologies to be developed, silicone devices can be put into widespread use without technologically limited delay.”
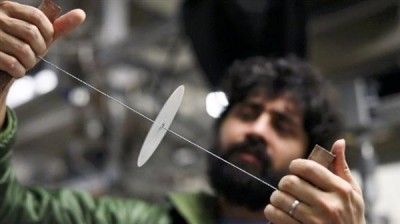
The new approach has brought the minimum features size for 3D printed silicone components down by somewhere between one to two orders of magnitude, the researchers say, opening up a host of new possibilities.
The group demonstrated robust tubes with walls just 450 micrometers thick and were able to print even finer structures, but the viscosity of the gel made it impossible to remove the delicate parts without damaging them.
They also demonstrated the ability to build a water pump that uses two free-floating balls inside two chambers as a series of valves that was printed in a single step. This ability to encapsulate something by 3D printing a chamber around it could also be applied to creating drug release devices.
Being able to print at such precision with a biocompatible material like silicone could not only make current medical implants stronger, less expensive, more flexible and more customizable, it could also make it possible to build more complex devices with complicated networks of valves and tubing. The ability of the printed materials to pump fluids and form thin-walled but strong tubes suggests it could also hold promise in creating prosthetics for everything from our airways to our digestive tracts.
Angelini’s group is still focusing on bioprinting in the long run, but this could prove a useful stopgap in the meantime.
Image Credit: Christopher O'Bryan/University of Florida